33a Myoora Road, Terrey Hills NSW 2084 | Tel 94608711 | Fax 94362103

Weight Loss (Bariatric) Surgery
Weight loss surgery is a powerful tool for patients struggling with obesity and associated illnesses such as diabetes, high blood pressure or sleep apnoea. The two most commonly performed weight loss surgery procedures are sleeve gastrectomy and gastric bypass.
Weight Loss Surgery
Weight loss surgery is performed as a laparoscopic (keyhole) procedure. Patients undergo weight loss surgery stay in hospital for two nights following their surgery.
All-inclusive packages for uninsured patients are available from $14,490.
IMPORTANT INFORMATION - READ BEFORE MAKING A BOOKING
Weight Loss Surgery Patient Information and Consent Form
Thank you for your interest in discussing weight loss surgery (WLS). It is important that you read this document prior to our initial consultation and have it with you at that time. Please make a note of any questions you have.
Undergoing WLS is an important decision, and it is important that you are well informed and understand the risks as well as the benefits.
The three most frequently performed weight loss operations in Australia are:
Laparoscopic Sleeve Gastrectomy. (SG)
Laparoscopic Roux-en Y gastric bypass. (RYGB)
Laparoscopic Mini Gastric Bypass. (MGB) also known as single anastomosis gastric bypass.
All operations are laparoscopic, (keyhole) with 5 small incisions, under general anaesthetic. Patients generally stay in hospital for 1-2 nights following surgery.
Most patients will opt for a Sleeve Gastrectomy however we will discuss the relative merits of each procedure at our consultation. Broadly speaking, Sleeve Gastrectomy is a more straightforward procedure with less complications than bypass surgery. Bypass operations are more effective against diabetes and may be more suitable for patients with pre-existing reflux symptoms.
Preparation prior to surgery
You will have at least consultation with me either in person or over the telephone. I will take a medical and surgical history and discuss the surgery with you. It is important that you ask any questions that you have.
You may also speak with our bariatric physician. Our bariatric physician will be able to answer many of your questions and will discuss any health problems you may have.
Some patients will see our perioperative physician and anaesthetist prior to surgery, particularly if they have a history of heart or lung problems, or diabetes that is difficult to control.
You will also have a consultation with one of our dietitians. Preoperative screening blood tests will be performed, and a good deal of information will be provided to you regarding the dietary preparation and implications of your surgery. You will need to be under the care of an experienced dietitian for the rest of your life, and you will need to undergo nutritional blood tests regularly. You may wish to continue your long-term care with our dietitian or another experienced bariatric dietitian.
Laparoscopic Sleeve Gastrectomy
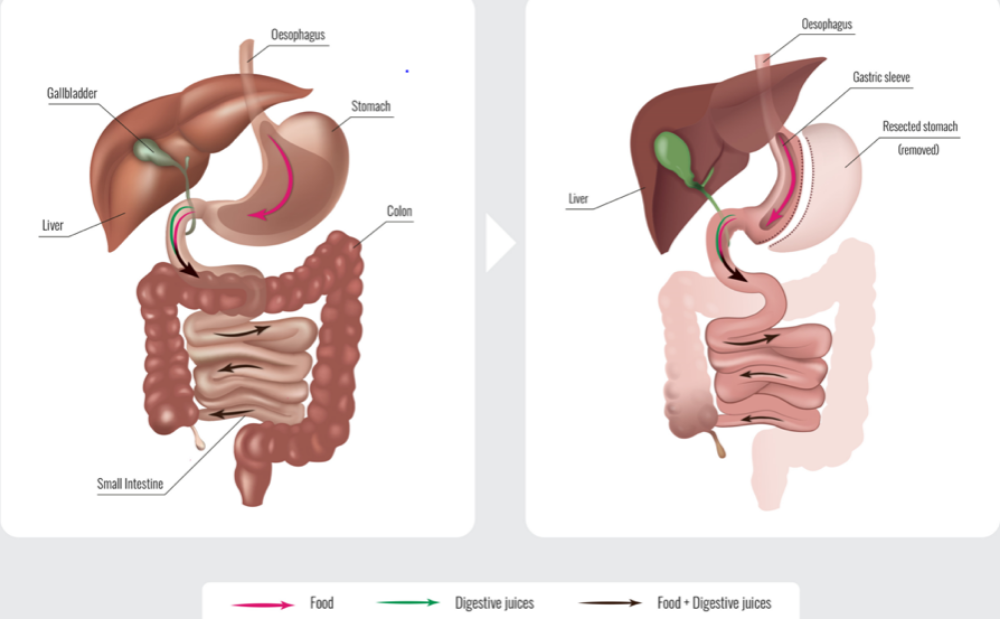
Laparoscopic sleeve gastrectomy involves removing most of the stomach leaving behind a narrow gastric (stomach) sleeve. This results in a decreased stomach capacity with patients feeling satiety (fullness) after a small meal.
Laparoscopic Roux-en-Y Gastric Bypass (RYGB)
Roux-en-Y gastric bypass involves dividing the stomach in two to form a gastric pouch. The small intestine is divided, and one end joined to the gastric pouch. Gastric secretions from the large portion of stomach as well as bile and pancreatic juices mixed with the food you eat downstream where the small intestine is joined to itself. This new arrangement results in patients feeling fuller after eating and influences the way fat, carbohydrate and nutrients are processed internally.
Laparoscopic Mini (one anastomosis) Gastric Bypass (MGB)
In the same way that early fullness is achieved in a Roux-en Y gastric bypass, the stomach is cut into two portions with a small pouch made from the top part of the stomach. In a mini gastric bypass, the intestine is joined directly to the stomach pouch without the formation of a “Y” shaped bypass. The advantages of this are thought to be a lower risk of surgical complications when compared to a Roux-en Y gastric bypass because the surgery itself is less complex.
Things to consider
Hiatus hernia and GORD
GORD (gastro-oesophageal reflux disease), or “reflux” is the feeling of acid rising up behind your breastbone and sometimes into your throat or mouth. GORD is common in the general community.
A hiatus hernia is a weakness in the diaphragm where the oesophagus passes through the diaphragm. Hiatus hernias may result in GORD.
I will ask you about reflux when we speak prior to your surgery. Some patients with bad reflux may decide to have a Roux-en-Y gastric bypass to prevent reflux worsening post-operatively. If a hiatus hernia is present at the time of your surgery, it will be repaired.
Fertility and Pregnancy
Weight loss from WLS results in increased fertility and the chances of getting pregnant. It is recommended that women do not fall pregnant for at least 12 months after WLS and until weight loss is stabilised. If you plan to fall pregnant soon after your WLS you should discuss this with your obstetrician before your WLS. You may wish to perform a pregnancy test prior to surgery
The oral contraceptive pill (OCP) may not be effective on the weeks following surgery. Use alternative methods of contraception during that time.
You should cease oestrogen containing contraception 1 month prior to WLS and use alternative methods of contraception. Oral contraception increases the risk of developing blood clots.
WLS may affect the effectiveness of the OCP in the long term, so you should discuss alternate measures of contraception with your GP.
Medications
You may need to make changes to your regular medications around the time of WLS.
Diabetes: Many diabetic medications will need to be ceased prior to your surgery. You should discuss all diabetic medications with me and the other doctors and dietitian in our clinic.
High Blood Pressure: Your blood pressure may decrease after your WLS. You should keep an eye on your blood pressure along with your GP in the weeks after your WLS. It may be that you need to decrease your blood pressure medications in the weeks after your WLS.
Blood thinners: You should discuss and blood thinner medication with me prior to your surgery. Most blood thinner medication will need to be ceased prior to surgery. It is fine to take aspirin around the time of your surgery. Some over the counter supplements and herbal medications thin the blood and should be ceased in the weeks before surgery.
Anti-inflammatory medication: You should cease anti-inflammatory medications around the time of your surgery. Generally, it is fine to recommence these medications after your surgery if you take anti acid medication to protect your stomach.
Surgery and Hospital Stay
You will be admitted to hospital on the day of surgery. You will meet the anaesthetist and myself in the operating theatres prior to your surgery. The total operating and anaesthetic time is usually around 1 ½ to 2 hours. Following the operation, you will go to the recovery ward and then to the surgical ward.
You will have an intravenous drip which will maintain your hydration. Drains and urinary catheters are not used routinely.
You will be encouraged to walk around the ward and increase gradually increase your fluid intake during your admission.
I will visit you during your hospital stay.
The abdominal incisions are closed with dissolving sutures that sit under the skin. The incisions will be dressed with waterproof dressings to enable showering. You should remove these one week after your surgery.
You will be given prescriptions for pain killers and anti-nausea medication to take home with you from the hospital. Take these as required.
You should also take acid suppression medication (Pantoprazole) for one month after your surgery in the case of sleeve gastrectomy and for 6 months in the case of bypass surgery. I will provide you with repeat prescriptions. This is to settle any reflux symptoms and prevent the development of ulcers.
After Surgery
You should resume your usual medications. You may need to decrease any diabetic or blood pressure medications as you lose weight. See notes above regarding medication.
Physical activity
You should modify your physical activity for a couple of weeks post operatively. You should not do any vigorous exercise or lift anything heavier than 10kgs for four weeks. You should not swim for two weeks following surgery.
You may drive when you are sufficiently comfortable and alert. This is usually around 5 days after your operation.
Patients doing sedentary or office work are usually able to return to work after 1 week to 10 days. Patients who do manual work may need to wait for 3 or 4 weeks prior to returning to work.
Nutrition
It’s very important that you continue to take vitamin supplements as directed by your dietitian and have regular blood tests to monitor your vitamin and mineral levels. You should see a dietitian regularly and have blood tests regularly.
The blood test guidelines are outlined below. You should show these guidelines to your dietitian and GP.
Bariatric surgery patients
Bariatric surgery patients should undergo yearly nutritional blood tests and 3 monthly if a deficiency is identified. They should take regular micronutrient supplements.
Patients should engage the services of an experienced dietitian and undergo lifelong nutritional assessment and monitoring. Routine monitoring should include Iron studies, B12 (active), Folate, Calcium, PTH, Vitamin D and Thiamine B1. Copper, Zinc, Vitamin A and E should also be measured in patients following a gastric bypass or those showing clinical signs of deficiency. Yearly monitoring of vitamin D, Calcium, PTH as well as a DXA/bone density scan is recommended in post-menopausal patients and those at risk of osteopenia/osteoporosis.
Complications
Serious complications following weight loss are very uncommon. Most patients will have a smooth postoperative recovery.
If you have any problems following your surgery, you should contact me without delay.
Potential complications include, but are not limited to:
General complications from abdominal surgery: Bleeding requiring blood transfusion or return to operating theatre (<1%) damage to other organs (<1%), deep venous thromboembolism or pulmonary embolism (<1%), serious infection (<1%) anaesthetic complications including heart or lung problems (<1%)
Nutritional complications: It is important that you take vitamin supplements as directed by your dietitian to avoid potentially serious problems with deficiency.
Weight Loss Surgery Complications:
Leak: a leak occurs when the internal stitching or stapling used in your surgery does not heal completely. This occurs in less than 1% of patients but may result in a prolonged hospital admission or further surgery.
Gastro-oesophageal reflux: This occurs in some sleeve gastrectomy patients and usually resolves. If not, patients may be required to take medication or undergo additional surgery.
Dumping and Changes in Bowel Function: These complications may occur after gastric bypass surgery. They usually resolve but may persist in some patients. Dumping may result in dizziness, palpitations sweating and diarrhoea.
Scarring and narrowing of the stomach or bowel.
Increased risk of gallstone formation, hair loss, food intolerance or changes in taste and smell.
Changes in psychological mood, Increased alcohol dependency, difficulty socialising due to small meal size.
Low blood pressure or low blood sugar which may require treatment with medication.

Please ask me if you would like to discuss any of these complications in more detail.
You will have follow-up appointments arranged with me and the other members of our team. Please don’t hesitate to contact me if you have any concerns. Further information regarding weight loss surgery is available at ifso.com
Other Conditions & Procedures
Hernia Surgery
Minimally invasive hernia repair restores abdominal strength and relieves discomfort.
Gallbladder surgery
Gallbladder removal is performed using keyhole surgery to relieve pain and prevent complications
Surgery for reflux (GORD)
Surgery for reflux strengthens the valve between the oesophagus and stomach to prevent acid reflux.
Surgery for large hiatus hernia
Keyhole surgery repairs the hiatus and returns the stomach to its normal position.
Laparoscopic and needlescopic surgery
Uses ultra-fine keyhole instruments to reduce pain and improve cosmetic outcomes.
Cancer surgery
Keyhole surgery is used to treat oesophageal and gastric cancers in combination with chemotherapy.